Diagrams courtesy of
Post-Polio Health International
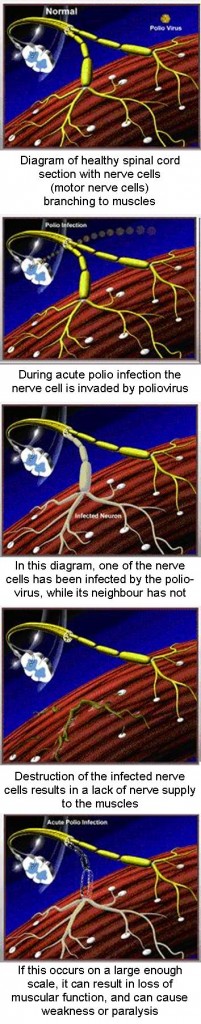
Acute poliomyelitis (polio, also known as 'infantile paralysis') is an anterior motor horn cell disease. During the initial acute infection, the polio virus infects spinal motor neurons and/or brainstem nuclei. This results in a widely variable distribution of weakness in skeletal and bulbar musculature, and residual impairment and paralysis ranging from minor muscle weakness to total paralysis requiring interventions such as ventilation.
Polio can strike at any age, but affects mainly children under three (over 50% of all cases). The virus enters the body through the mouth and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck and pain in the limbs. One in 200 infections leads to irreversible paralysis (usually in the legs). Amongst those paralysed, 5%-10% die when their breathing muscles become immobilized. Although polio paralysis is the most visible sign of polio infection, fewer than 1% of polio infections ever result in paralysis. Poliovirus can spread widely before cases of paralysis are seen. As most people infected with poliovirus have no signs of illness, they are never aware they have been infected. After initial infection with poliovirus, the virus is shed intermittently in faeces (excrement) for several weeks. During that time, polio can spread rapidly through the community.
Who is most at risk from polio?
Polio mainly affects children under five years of age. However, immune and or partially immune adults and children can still be infected with poliovirus and carry the virus for long enough to take the virus from one country to another, infecting close contacts and contaminating sanitation systems. This could facilitate transmission especially in countries where sanitation systems are sub-standard.
How is polio spread?
In the remaining polio endemic countries, poliovirus is mainly passed through person-to-person contact. Most people infected with the poliovirus do not develop polio paralysis or other symptoms of polio infection. However one in 200 people do have symptoms and can become paralyzed. The virus enters the environment through faeces of people infected then is passed to others especially in situations of poor hygiene. The poliovirus can also infect persons who have been vaccinated and can be carried by them. Such individuals will not develop polio, but can carry the virus in their intestines and can pass it to others in conditions of sub-standard hygiene. The disease may infect thousands of people, depending on the level of sanitation, before the first case of polio paralysis emerges. Individuals can carry the virus in their intestines just long enough to transmit to others. WHO considers a single confirmed case of polio paralysis to be evidence of an epidemic - particularly in countries where very few cases occur.
How can polio be prevented?
There is no cure for polio, it can only be prevented through immunisation. Polio vaccine, given multiple times, almost always protects a child for life. Full immunisation will markedly reduce an individual's risk of developing paralytic polio. Full immunisation will protect most people, however individuals can still contract the disease due to the failure of some individuals to respond to the vaccine.
Polio paralysis
Once established in the intestines, poliovirus can enter the blood stream and invade the central nervous system - spreading along nerve fibres. As it multiplies, the virus destroys nerve cells (motor neurons) which activate muscles. These nerve cells cannot be regenerated and the affected muscles no longer function. The muscles of the legs are affected more often than the arm muscles. The limb becomes floppy and lifeless - a condition known as acute flaccid paralysis (AFP). More extensive paralysis, involving the trunk and muscles of the thorax and abdomen, can result in quadriplegia. In the most severe cases (bulbar polio), poliovirus attacks the motor neurons of the brain stem - reducing breathing capacity and causing difficulty in swallowing and speaking. Without respiratory support, bulbar polio can result in death.
The iron lung

June Middleton (1926 - 2009) spent 60 years
in an iron lung (Victoria, Australia)
Large polio epidemics caused panic every summer during the 1940s and 50s in industrialised countries. At that time, people with polio affecting the respiratory muscles were immobilized inside "iron lungs" - huge metal cylinders that operated like a pair of bellows to regulate their breathing and keep them alive. Today, the iron lung has largely been replaced by the positive pressure ventilator; nevertheless, it is still in use in some countries. This page contains glimpses into life in an iron lung, told by the polio survivors themselves.
Children whose legs are paralysed by polio today often require crutches, special braces or wheelchairs in order to move around.
Because no drug developed so far has proven effective, treatment is entirely symptomatic. Moist heat is coupled with physical therapy to stimulate the muscles and antispasmodic drugs are given to produce muscular relaxation. While this can improve mobility, it cannot reverse permanent polio paralysis.
Source: www.polioeradication.org


